


DIGITAL BIOTHESIOMETRY
Diabetic neuropathy is usually diagnosed based on your symptoms, your medical history and a physical exam. Loss of sensation due to Neuropathy is the major cause of painless injuries to the feet. Such injuries result into chronic ulcerations and complications leading to large amputations. Hence, early and accurate detection of sensation loss due to neuropathy is the best way to protect the feet from amputation. Also, it is very important to quantify sensation loss risk to monitor the trend by follow up. The Digital Vibratory Perception Threshold at various sites on planter foot quantifies the loss of sensation. Increase in VPT means diminished sensation and increasing risk. Biothesiometer is a digital electronic tuning fork system with computer interface. This simple to use quantitative tools helps to diagnose the loss of sensation and grades the diabetic neuropathy.
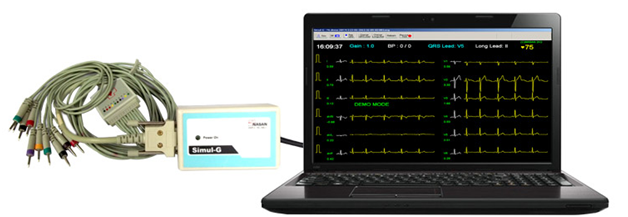
Computerized Electrocardiogram (ECG)
An electrocardiogram (ECG) is an electrical recording of the heart and is used in the investigation of heart disease. An ECG shows the heart's electrical activity as line tracings on paper. Patients with diabetes have a very high incidence of silent but medically significant coronary artery disease. Coronary artery disease remains the leading cause of premature morbidity or mortality for patients with diabetes mellitus. Compared to people without diabetes, people with type 1 and type 2 (especially women) are at higher risk of developing heart disease, and at an earlier age. Unfortunately, a large proportion will have no symptoms before either a fatal or a nonfatal myocardial infarction (MI). Hence, it is desirable to identify patients at high risk for vascular events, especially patients with established severe coronary artery disease (CAD).
Computerized Fundus Examination for DIABETIC RETINOPATHY

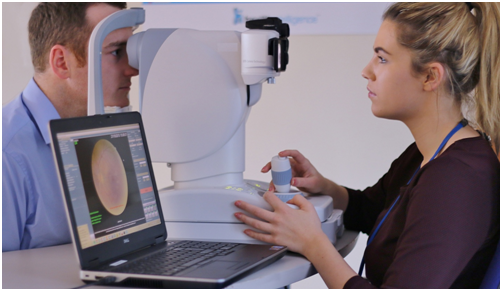
Diabetic retinopathy is the most common form of diabetic eye disease. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. Diabetic retinopathy is a serious sight-threatening complication of diabetes. Symptoms of diabetic retinopathy include seeing spots or floaters, blurred vision, having a dark or empty spot in the center of your vision, difficulty seeing well at night. Patients with diabetes who can better control their blood sugar levels will slow the onset and progression of diabetic retinopathy. Often the early stages of diabetic retinopathy have no visual symptoms. That is why everyone with diabetes should undergo a comprehensive eye examination once a year. Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy. This test is done at Diabelife.

Glucometer
A blood glucose meter is a small, portable machine that's used to measure the blood glucose level. These work by analyzing a small amount of blood, usually from a fingertip. The glucometer lightly pricks your skin to obtain the blood. People with diabetes often use a blood glucose meter to help them manage their condition. Using a blood glucose meter can help you better manage your diabetes by tracking any fluctuations in your blood glucose level. If you have diabetes, monitoring your blood glucose level provides you and your doctors with valuable information about how food, exercise, medications, stress, and other factors affect your blood glucose. This information will help you and your doctor construct a treatment plan tailored to your needs. Know Your Blood Sugar Numbers: Use glucometer to Manage Your Diabetes. Keeping track of your blood glucose can help you and your doctor make a plan to manage this condition. Meters tell you your current blood sugar, but since blood sugar levels change, you need to test levels often and record them. Meters and their test strips vary in cost and size. They also vary by functions and features.
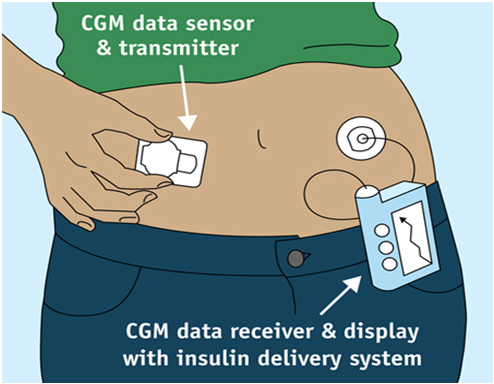
Continous Glucose Monitor
Continous Glucose Monitoring (CGM) is a way to measure glucose levels in real time throughout the day and night notifying you of high sugar levels and low sugar levels that will help your diabetologist to take action. A tiny electrode called a glucose sensor is inserted under the skin to measure glucose levels in tissue fluid. The glucose sensor produces an electronic signal that is related to the amount of glucose present in the blood. It is connected to a transmitter that sends that information to the data monitoring device using radio frequency. The transmitter is waterproof and can be worn while swimming, bathing, or showering without worries. Unlike blood glucose meter, which provides just a single glucose reading, CGM system provides real-time, dynamic glucose information every 30 minutes in a 24-hour period and for 7 days. This gives valuable insight about your glucose levels, speed, and direction and valuable insight to your diabetologist to proactively managing your diabetes. A blood glucose meter only provides “snapshot” of your glucose level at a single moment in time. In contrast a CGM device gives you a greater view of your glucose trends for 5- 7 days. CGM can be used by Type 1, Type 2, and gestational diabetes patients who would like better glucose control to improve the health and quality of their lives.

Insulin Pump
An insulin pump is a small, computerized device that delivers insulin continuously throughout the day via a catheter placed under the skin. Because the insulin pump stays connected to the body, it allows the wearer to modify the amount of insulin they take within the press of a few buttons at any time of the day or to program in a higher or lower rate of insulin delivery to occur at a chosen time, which can be when sleeping. An insulin pump consists of the main pump unit which holds an insulin reservoir which is attached to a long, thin piece of tubing with a needle or cannula at one end. The most modern trend in insulin pump technology is for pumps to directly interact with CGMs. Insulin pumps are connected to the body via the infusion set. The small needle or plastic cannula sits under your skin through the day whilst the infusion set is held in place by an adhesive that is similar to the sticky backing of a plaster. It is also known as continuous subcutaneous insulin infusion (CSII). Insulin pump therapy has been recognised as being effective in helping people with diabetes, particularly people with type 1diabetes, to achieve improved HbA1c levels helping them to improve quality of life.
Hand Held Doppler
Hand held Doppler examination is a frequently used non-invasive vascular assessment utilised by diabetologists/ podiatrists. Doppler studies have an essential role to play in the investigation of peripheral vascular disease. It is small, highly portable and easy to use. It allows quick identification of patients without significant peripheral vascular disease and those requiring further investigation. It can be also has applications in the assessment of venous disease. The hand-held Doppler unit is now widely used in clinical practice by many health professionals to assess blood flow in peripheral vessels.


Ambulatory Blood Pressure Monitoring (ABPM)
Ambulatory blood pressure (ABP) monitoring involves measuring blood pressure (BP) at regular
intervals (usually every 20–30 minutes) over a 24 hour period while patients undergo normal daily activities, including sleep. ABPM is safe and is not usually associated with complications. Blood pressure is measured over a 24-hour period, using auscultatory or oscillometry devices, and requires use of a cuff. The monitor takes blood pressures every 30 minutes or as programmed. Ambulatory BP monitoring provides a more reliable measure of a patient’s BP than isolated clinic measures and is not subject to the ‘white-coat effect’ or White coat hypertension.
Who should be referred for ambulatory blood pressure monitoring?
• The National Institute for Health and Care Excellence (NICE) recommends that if a clinic blood pressure is 140/90 mm Hg or higher, ABPM should be offered to confirm the diagnosis of hypertension.
• Poorly controlled hypertension - eg, suspected drug resistance.
• Patients who have developed target organ damage despite control of blood pressure.
• Patients who develop hypertension during pregnancy.
• High-risk patients - eg, those with diabetes mellitus, those with cerebrovascular disease, and kidney transplant recipients.
• Suspicion of white coat hypertension - high blood pressure readings in clinic which are normal at home.
• Suspicion of reversed white coat hypertension, ie blood pressure readings are normal in clinic but raised in the patient's own environment.
• Postural hypotension.
• Elderly patients with systolic hypertension.
Diabetic Footwear
Taking good care of your feet means making sure you have the right foot wear. Proper footwear is an important part of an overall treatment program for people with diabetes, even for those in the earliest stages of the disease. If there is any evidence of neuropathy, or lack of sensation, wearing the right footwear is crucial. By wearing special footwear, many patients can prevent serious diabetic foot complications. A properly fitting shoe made of soft materials like MCR or MCP with a shock absorbing sole may be all that you need. It is also important for patients to learn how to select the right type of shoe in the right size, so that future problems can be prevented. The excessive pressure and friction from the wrong kind of shoes or from poorly fitting shoes can lead to blisters, calluses and ulcers. Many diabetics need special footwear prescribed by a physician. Wearing specially designed shoes can help reduce risk and promote healthy circulation in your feet.
If you have diabetes, you should avoid wearing certain types of shoes
• Avoid any shoe with a pointed toe because it will aggravate your toes and restrict circulation.
• Don’t wear shoes without arch support, as they may lead to the breakdown of tissue in your foot.
• Be careful to avoid shoes that don’t fit properly, as those could injure your feet.
• Wear high heels sparingly it all. If you do wear high heels, round-toe styles with heels below 2 inches are best.
